PrEP for Adults
Implementation Forum, August 26, 2015
This forum, held on August 26th, 2015, was the first of a series of four statewide PrEP Implementation forums that brought together a wide variety of stakeholders from across the state. This forum was attended by healthcare providers, consumers, community stakeholders, and state and local health officials to discuss the use of PrEP and PrEP quality of care for adults in New York State.
The summary report of this event is divided into three parts. Part one is an overview of panel presentations given by providers in different health care settings currently implementing PrEP in pilot programs. Part two summarizes recommendations provided by participants on four key topics related to PrEP implementation at the forum: quality metrics, implementation, policy, and the intersection of PrEP and sexually transmitted infections (STIs). Part three discusses the next steps that will be executed to implement the recommendations outlined in this report.
Meeting Materials
Summary Report
August 2015
This report summarizes speaker presentations and the panel and participant discussions at the first statewide forum on implementation of pre-exposure prophylaxis (PrEP) for adults, which was hosted by the New York State Department of Health AIDS Institute (NYSDOH AI) on August 26, 2015.
Agenda with Links to Slides
- Welcome and Review of Agenda: Bruce Agins, Medical Director, Office of the Medical Director, NYSDOH AIDS Institute
- Opening Remarks: Dan O’Connell, Director, NYS DOH AIDS Institute, and Demetre Daskalakis, MD, MPH, Assistant Commissioner, Bureau of HIV/AIDS Prevention and Control, NYC DOHMH
- Keynote Speaker: Ken Mayer, The Fenway Institute
NYS PROVIDER PRESENTATIONS
- Dan O’Connell, Director, NYS DOH AIDS Institute
Pre-Exposure Prophylaxis (PrEP) Initiatives in New York State: A Brief Overview | View Slides - Demetre Daskalakis, MD, MPH, Assistant Commissioner, Bureau of HIV/AIDS Prevention and Control, NYC DOHMH
NYC and PrEP | View Slides - Kenneth H Mayer, MD, Medical Research Director, Co-Chair, The Fenway Institute
The Fenway Institute: PrEP Update | View Slides - Shona Ruggeri, PrEP Coordinator, Designated AIDS Center, Albany Medical Center
Overview of Albany Medical Center’s PrEP Program | View Slides - Michael Lee, Senior Director of Business Development, Evergreen Health Services
Evergreen Medical Group, Buffalo, NY: PrEP Program | View Slides - Jeffrey M Birnbaum, MD, MPH, Executive Director, HEAT Program, SUNY Downstate Medical Center
HIV Pre-Exposure Prophylaxis Panel | View Slides - Robert Murayama, MD, MPH, Chief Medical Officer, Apicha Community Health Center
Apicha Community Health Center: PrEP | View Slides - Luis Freddy Molano, MD, Vice President of Infectious Diseases and LGBTQ Programs and Services, Community Healthcare Network
PrEP through the Sexual and Behavioral Health Program | View Slides - Michel Ng, NP and Joaquin Aracena, MA, Mount Sinai Hospital
PrEP Panel | View Slides - William M Valenti, MD, Senior Vice President for Organizational Advancement, Co-Founder, and Staff Physician, Trillium Health
PrEP: An Organizational Initiative | View Slides - Peter Meacher, MD, FAAFP, AAHIVS, Chief Medical Officer, Callen-Lorde Community Health Center
Pre-Exposure Prophylaxis | View Slides
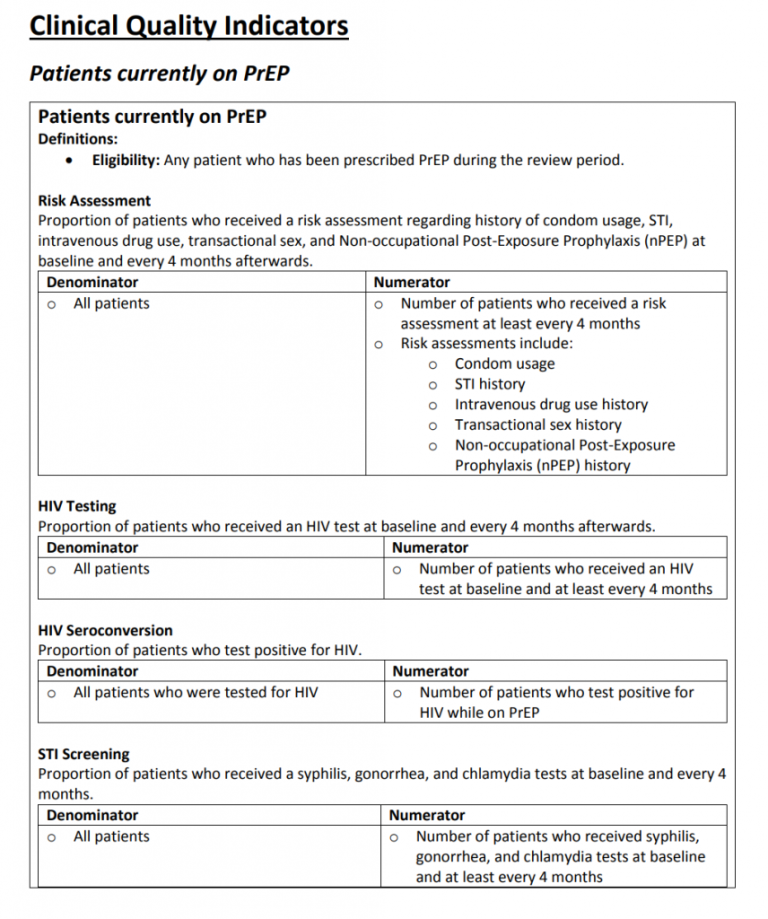
Clinical Indicators for PrEP
Click here to download the full Clinical Quality Indicators for patients currently on PrEP.
PrEP for Adolescents

Welcome
The New York State Department of Health AIDS Institute convened the first statewide forum on adolescent PrEP implementation to bring together stakeholders from across the State to discuss the unique issues associated with providing pre-exposure prophylaxis (PrEP) for adolescents engaged in high-risk behaviors.
The forum invited PrEP providers, public health officials, and community members representing a wide variety of perspectives to contribute insights stemming from their experiences with delivering PrEP services to adolescents in diverse settings. The discussion focused on identifying successes to date; policy issues and clinical practice challenges in delivering PrEP to adolescents; and opportunities for change to expand PrEP for adolescents statewide in support of the NYS End the Epidemic by 2020 Initiative.
Meeting Materials
Speaker Presentations
- Dan O’Connell, Director, NYS DOH AIDS Institute
Opening Remarks | View Slides
- Demetre Daskalakis, MD, MPH, Assistant Commissioner, Bureau of HIV/AIDS Prevention and Control, NYC DOHMH
Opening Remarks (Dr. Daskalakis did not present slides) - Bill Kapogiannis, MD, Adolescent Medicine Trials Network for HIV/AIDS Interventions, National Institutes of Health
ATN 110: An HIV PrEP Demonstration Project and Phase II Safety Study for Young MSM in the US | View Slides - Susan Rosenthal, PhD, ABPP, Director, Division of Child and Adolescent Health, Columbia University Adolescent
Autonomy and Decision-Making: Implications for Prescribing PrEP | View Slides - Lillian Rivera, MPH, The Center for LGBTQ Youth Advocacy and Capacity Building, Hetrick-Martin Institute
Imagining a Tomorrow with Choices: Mapping a Trajectory for YMSM Access to PrEP Based on the History of Reproductive Justice | View Slides
Panel Discussion: Implementation in an Adolescent PrEP Clinic
- Donna Futterman, MD, Adolescent AIDS Program, Children’s Hospital at Montefiore
View Slides
- Jeff Birnbaum, MD, Heat Program, SUNY Downstate
View Slides
- David Rosenthal, DO, PhD, Center for Young Adult, Adolescent and Pediatric HIV, North Shore-LIJ Medical Group
View Slides - Uri Belkind, MD, MS, Health Outreach to Teens (HOTT), Callen-Lorde
View Slides
Summary Report
December 2015

This report summarizes speaker presentations and the panel and participant discussions at the first statewide forum on implementation of pre-exposure prophylaxis (PrEP) for adolescents, which was hosted by the New York State Department of Health AIDS Institute (NYSDOH AI) on November 18, 2015.
Speaker Bios
Uri Belkind, MD, MS
Dr. Belkind is an Adolescent Medicine physician and pediatrician. Originally from Mexico, he obtained his medical degree, at the Universidad Nacional Autonoma de Mexico. He completed his residency in Pediatrics at Jackson Memorial Hospital, University of Miami, where he served as Chief Resident, and was later accepted as a post-doctoral fellow in Adolescent Medicine at Montefiore Medical Center. Uri is currently the Clinical Director of the Health Outreach to Teens (HOTT) program at Callen-Lorde Community Health Center in New York City, a comprehensive, multi-disciplinary program designed specifically to meet the medical and mental health needs of lesbian, gay, bisexual, transgender, and questioning adolescents and young adults ages 13-24.
Jeffrey Birnbaum, MD
Dr. Birnbaum is an Associate Professor of Pediatrics and Public Health at SUNY Downstate Medical Center and currently serves as the Principal Investigator and Executive Director of the Health & Education Alternatives for Teens (“HEAT”) Program. HEAT is the only program of its kind in Brooklyn to offer comprehensive medical and mental health care, supportive services, and access to clinical research for HIV+ and at-risk youth, aged 13 to 24. At HEAT, he has provided medical care to hundreds of HIV+ youth ages 13-24 years since 1992. Dr. Birnbaum is an adolescent medicine specialist and Board certified pediatrician who has devoted most of his professional career working with HIV+ youth. Today, HEAT operates a “one-stop” full service clinic, offering a full range of developmentally appropriate and culturally competent medical, mental health and supportive services that are tailored to meet the special health care needs of young people at very high risk for HIV. In addition to his clinical work at HEAT, he devotes much of his time in community mobilization efforts to identify and engage HIV+ youth in care. He has pioneered efforts in Brooklyn to engage young gay, bisexual male youth and transgender youth in medical care, prevention activities and HIV counseling and testing efforts. Through his efforts, Dr. Birnbaum has provided this particular community of young people in Brooklyn access to health care that lessens the huge health disparities they face. Dr. Birnbaum has also been a pioneer in the realm of transgender health. As a result of his efforts, HEAT operates the only transgender health clinic for youth, ages 13-24 years, in Brooklyn. His advocacy for the rights of transgender youth to be able to access hormonal therapy has been recognized both locally and nationally.
Demetre Daskalakis, MD, MPH
Dr. Daskalakis is the Assistant Commissioner of the Bureau of HIV Prevention and Control of the NYC Department of Health and Mental Hygiene. He received his medical education from NYU School of Medicine and completed his residency training in 2003 at Beth Israel Deaconess Medical Center in Boston. He also completed Clinical Infectious Disease fellowships at the Brigham and Women’s | Massachusetts General Hospital combined program. He received his Masters of Public Health from the Harvard School of Public Health. He has been a career-long physician activist in the area of HIV treatment and prevention among LGBT people.
Donna Futterman, MD
Dr. Futterman is a Professor of Clinical Pediatrics and the Director of the Adolescent AIDS Program at Montefiore in the Bronx New York. Her program was the first in the nation to offer comprehensive care to HIV+ youth and continues as one of the largest. The program is funded by research, clinical, educational and outreach grants. While continuing to serve HIV+ youth, the program has expanded its funding to provide care to at-risk youth, especially LGBT youth offering: care, support, hormones, PEP and PREP. Dr. Futterman is recognized as a local and international advocate for youth (and has written over 80 articles and chapters).
Bill G. Kapogiannis, MD, FAAP
Dr. Kapogiannis joined the Maternal and Pediatric Infectious Disease Branch (MPIDB) in July 2005. He is a board-certified infectious-disease specialist in both pediatrics and internal medicine. He received his M.D. from the University of Illinois at Chicago College of Medicine and completed a four-year internal medicine/pediatrics residency program at the University of Illinois at Chicago before finishing a combined fellowship training in infectious diseases within the departments of Internal Medicine and Pediatrics at Emory University, Atlanta, Georgia. At the NIH, Dr. Kapogiannis’ research is focused on HIV in adolescents; he is the scientific director of the Adolescent Trials Network for HIV/AIDS Interventions (ATN), which is evaluating biomedical, behavioral, and community level interventions along the entire continuum of care for treatment and management of HIV infection and its complications among youth, as well as the prevention of HIV transmission in the adolescent population, including HIV vaccine, microbicide and pre-exposure prophylaxis (PrEP) studies. He is also the primary NIH Scientific Collaborator on and the IND sponsor of ATN’s Project PrEPare (ATN 110 and ATN 113 PrEP studies among young MSM in the US).
Dan O’Connell
Mr. O’Connell is the Director of the New York State Department of Health AIDS Institute. Dan recently celebrated his 30 year anniversary in State service. During his years of service Dan has consistently led efforts to revise and revitalize programming and state laws for HIV, STD, HCV, LGBT health and drug user health. Over the last two years, he has worked with community stakeholders on a process that resulted in a Governor endorsed effort to bring HIV below epidemic levels in NYS by the end of 2020. Dan is an Executive Committee member of the National Alliance of State & Territorial AIDS Directors, chairs the NYS Interagency Task Force on AIDS, and in 2014 received an award from the White House for his work in hepatitis.
Lillian Rivera
Ms. Rivera has a decade’s worth of experience in youth development, and is currently the Director of Advocacy and Capacity Building at the Hetrick-Martin Institute (HMI), the nation’s oldest and largest LGBTQ youth serving agency with sites in New York City and Newark New Jersey. Ms. Rivera has appeared on numerous media outlets including Cristina, CNN en Español and NBC Latino, offering her expertise on best practice in working with LGBTQ youth. She has had articles on her work with LGBTQ youth and her life as a Latina Lesbian Mom published on the Huffington Post and the Feminist Wire. Prior to assuming the role of Director of Advocacy and Capacity Building, Ms. Rivera served as Director of After-School Services, managing the largest direct service area at the Hetrick-Martin Institute. She received her BA in Theatre and MPH from Rutgers University.
David Rosenthal, DO, PhD
Dr. Rosenthal is the Medical Director for the Center for Young Adult Adolescent and Pediatric HIV at North Shore-LIJ Health System; his office is in Great Neck, Long Island. The Center for Young Adult, Adolescent and Pediatric HIV has grant funding from the NYS DOH AIDS Institute, HRSA Ryan White Part D, and is also supported by a grant from the CDC. Recently, in addition to focusing on care of adolescents and young adults living with HIV, Dr. Rosenthal has been addressing LGBTQ inclusion in health care, and HIV prevention. He has opened a satellite clinic at Pride for Youth in Long Island providing low threshold medical care including screening for PrEP.
Susan Rosenthal, PhD, ABPP
Dr. Rosenthal is the Director of the Division of Child and Adolescent Health and the Vice Chair of Faculty Development within the Department of Pediatrics. Her research focuses on the areas of adolescent health, specifically the promotion of sexual health and vaccine acceptability from a developmental perspective. Her current R01 focuses on adolescent and parents attitudes towards research participation and willingness to participate in reproductive health clinical trials. Dr. Rosenthal also has an interest in the development of leadership skills, the issues in mentoring in diverse relationships, and the use of faculty reviews to promote the growth of the faculty and the department.
Agenda with Links to Slides
- Welcome & Introductions: Lyn Stevens, MS, NP, ACRN, Deputy Director, Office of the Medical Director, NYS DOH AIDS Institute
- Opening Remarks: Dan O’Connell, Director, NYS DOH AIDS Institute | View Slides
- Opening Remarks: Demetre Daskalakis, MD, MPH, Assistant Commissioner, Bureau of HIV/AIDS Prevention and Control, NYC DOHMH (Dr. Daskalakis did not present slides)
PART I: INVITED SPEAKERS
- ATN 110: An HIV PrEP Demonstration Project and Phase II Safety Study for Young MSM in the U.S. | View Slides
Bill Kapogiannis, MD, Adolescent Medicine Trials Network for HIV/AIDS Interventions, National Institutes of Health - Adolescent Autonomy and Decision-Making: Implications for Prescribing PrEP | View Slides
Susan Rosenthal, PhD, ABPP, Director, Division of Child and Adolescent Health, Columbia University - Imagining a Tomorrow with Choices: Mapping a Trajectory for YMSM Access to PrEP Based on the History of Reproductive Justice | View Slides
Lillian Rivera, MPH, The Center for LGBTQ Youth Advocacy and Capacity Building, Hetrick-Martin Institute - Questions and Answers
WORKING LUNCH WITH PANEL DISCUSSION: PrEP Implementation in an Adolescent PrEP Clinic
- Donna Futterman, MD, Adolescent AIDS Program, Children’s Hospital at Montefiore | View Slides
- Jeff Birnbaum, MD, Heat Program, SUNY Downstate | View Slides
- David Rosenthal, DO, PhD, Center for Young Adult, Adolescent and Pediatric HIV, North Shore-LIJ Medical Group | View Slides
- Uri Belkind, MD, MS, Health Outreach to Teens (HOTT), Callen-Lorde | View Slides
- Questions and Answers
ROUND ROBIN BREAKOUT SESSIONS
Participant Discussions: Attendees will circulate through three 25‐minute breakout sessions to discuss their experiences with the following key topics in adolescent PrEP implementation: consent, payment, retention, adherence, sexual health, and clinical care. After 25 minutes of discussion in one session, participants will be directed to the next session until everyone has had the opportunity to participate in each of the 3 sessions. After a short break, we will gather to report out and identify priorities for policy and change.
PRIORITIES FOR POLICY CHANGE AND REPORTS FROM BREAKOUT SESSIONS
Report Out: Successes, Challenges & Priorities for Change: Session leaders will report out to the whole group with the goal of identifying the top 3‐5 items in each of the following areas:
- Issues and challenges unique to PrEP implementation for adolescents
- Keys to success, including best practices for engaging adolescents
- Policies needed to increase adolescent access to PrEP statewide
- Priorities for change to guarantee success in the next 3 years
Next Steps & Closing Remarks: Lyn Stevens
Resources
- AIDS Institute Guidance for the Use of PrEP to Prevent HIV Transmission
- Ending the AIDS Epidemic in New York State
- NYCDHMH PrEP Information
- NYCLU Reference Card on Minors’ Rights to Confidential Reproductive & Sexual Health Care in New York
- NYSDOH PrEP and PEP Information
- NYSDOH PrEP Assistance Program
- PrEP Use among Sexually Active Adolescents: Consultation on Clinical, Ethical and Operational Considerations for the implementation of Oral Pre-Exposure Prophylaxis (PrEP) in Sexually Active Older Adolescents (15 – 19) at High Risk of HIV Infection, HIV Section, UNICEF New York, July 2015
PrEP for Women
Posted October 18, 2017
This forum was the third in a series and a continuation of efforts to engage community and policy stakeholders in support of Governor Andrew Cuomo’s plan to end the HIV epidemic in New York State. A key component of the governor’s plan is to increase access to and uptake of PrEP among people who are at high risk of acquiring HIV infection.
PrEP implementation for adults was addressed on August 26, 2015, when the New York State Department of Health AIDS Institute (NYSDOH AI) convened a forum, attended by healthcare providers, consumers, community stakeholders, and state and local health officials, to discuss the use of PrEP and PrEP quality of care for adults in New York State. On November 18, 2015, a forum on implementation of adolescent PrEP was convened to address challenges and opportunities specific to the youth population. This forum on PrEP for women focused on identifying challenges that must be addressed to increase women’s access to PrEP and their willingness to use it to protect themselves from acquiring HIV.
Available meeting materials:
- Meeting Summary Report
- Agenda
- Speaker Presentations (links to slides)
- Speaker Bios
- Breakout Session Guidance
Challenges Unique to Women
Among presenters, panelists, and meeting participants, there was broad agreement that women in New York State are particularly vulnerable to HIV infection due to a mix of social, behavioral, and biological factors. In New York State, in 2015, 20% of new HIV diagnoses were in women, and nearly all reported their transmission risk as heterosexual contact [1].
In New York, women of color and particularly Black women, have been disproportionately affected by HIV. In 2015, 59% of all new HIV diagnoses in women were in Black women, who comprise only 16% of the total female population. Research in New York City demonstrated that few women know about PrEP, and very few are using this prevention intervention.
Key Issues
All agreed that barriers to PrEP uptake fall into three domains: awareness, attitudes, and access.
- Lack of awareness: Neither women nor their care providers know much about PrEP. Care providers who don’t know about PrEP, or who don’t know how to prescribe it, cannot offer or engage women in discussions of or education about PrEP. Women who don’t know about it or who have only seen PrEP marketed to gay men will not know or think to ask about this prevention method. Care providers are also subject to the same messaging as women and may mistakenly believe that PrEP is for gay men, not women.Priority for Change: All agreed that education and training are needed for clinical and non-clinical care providers so that all providers who deliver care to women can inform women about PrEP and provide access.
- Attitudes: Many care providers still focus on a “risk assessment” approach to HIV prevention intervention. This focus can be stigmatizing with its emphasis on identifying “risky” or “bad” behaviors that may expose a woman to HIV.Priority for Change: Shifts in attitude are needed among healthcare providers, who must take the first steps toward promulgating a view of PrEP as an essential component of women’s health and a routine part of healthcare for women.
- Access: Access starts with care providers—a care provider who does not know about PrEP and understand its role in sexual health cannot offer PrEP to women; therefore, access depends on increasing awareness. But access also depends on delivery—PrEP should be made available in as many settings as possible and on demand, and there should be adequate resources available to help women cover the costs of PrEP prescriptions and related expenses.Priority for Change: Expanded education is needed, in a greater number of settings and types of settings where PrEP is prescribed, and expanded resources are needed to provide PrEP to women at reduced or no cost.
- “Female Sex Assigned at Birth, Newly Diagnosed with HIV Infection by Age at Diagnosis and Transmission Risk Category, NYS, 2015”. Bureau of HIV/AIDS Epidemiology, AIDS Institute, NYSDOH.
Summary Report
Posted October 18, 2017
This report summarizes speaker presentations and panel and participant discussions at the first statewide forum on PrEP implementation for women in New York. This meeting was hosted by the New York State Department of Health AIDS Institute (NYSDOH AI) on June 8, 2017.
Speaker Bios
Posted October 18, 2017
Kate Collier, MPH, PhD
Dr. Collier is the Director of Research and Evaluation at Planned Parenthood of New York City. In this role, she conducts research to support new agency initiatives and serves as the evaluator for PPNYC’s Project Street Beat program. Kate has previously worked for the HIV Center for Clinical and Behavioral Studies at Columbia University and the NYS Psychiatric Institute, the Columbia University Mailman School of Public Health, and Gay Men’s Health Crisis. She holds a PhD in social sciences from the University of Amsterdam.
Demetre Daskalakis, MD, MPH
Dr. Daskalakis is the Deputy Commissioner for the Division of Disease Control at the New York City Department of Health and Mental Hygiene. Dr. Daskalakis directs the public health laboratory and all infectious disease control programs for New York City, including HIV, tuberculosis, STIs, vaccine-preventable diseases, and general communicable diseases. His division is one of the largest in the Department, employing more than 1,000 staff, managing >$350 million, and operating 17 clinical facilities. He received his medical education from NYU School of Medicine and completed his residency training in 2003 at Beth Israel Deaconess Medical Center in Boston. He also completed Clinical Infectious Disease fellowships at the Brigham and Women’s/Massachusetts General Hospital combined program. He received his master’s degree in public health from the Harvard School of Public Health. He has been a career-long physician-activist in the area of HIV treatment and prevention among LGBTQ+ people.
Dázon Dixon Diallo, MPH, DHL
Dr. Diallo is an advocate in the struggle for women’s human rights and reproductive justice and the fight against HIV/AIDS, on behalf of communities of women living with HIV and those at risk of HIV and STIs. In 1989, Diallo founded SisterLove, Inc., the first women’s HIV/AIDS and RJ organization in the southeastern United States. She is a member of In Our Own Voice: The National Black Women’s Reproductive Justice Agenda, where she advocates for sexual and reproductive justice in public health and prevention policies and programs. Diallo is a member of the Board of Directors of the National Women’s Health Network, is a founding member of the 30 for 30 Campaign for Women in the National HIV AIDS Strategy, serves on the Fulton County HIV Advisory Board and is a co-chair for the Act Now End AIDS national coalition. She was recently appointed to the National Institutes of Health Office on AIDS Research Advisory Council. Dr. Diallo holds a master’s degree in public health from the University of Alabama at Birmingham and bachelor’s degrees from Spelman College. In 2012, Diallo received an honorary doctorate of Humane Letters from her alma mater, Spelman College. She convenes the only national coalition of women focused on HIV and biomedical prevention, the U.S. Women & PrEP Working Group.
Betsy C. Herold, MD
Dr. Herold is Professor of Pediatrics and Microbiology-Immunology; Vice Chair for Research in the Department of Pediatrics; and Division Chief, Pediatric Infectious Diseases at Albert Einstein College of Medicine and the Children’s Hospital at Montefiore in the Bronx, NY. Dr. Herold graduated from the University of Pennsylvania Medical School and completed a residency in pediatrics, clinical fellowship in pediatric infectious diseases, and postdoctoral fellowship in herpes virology at Northwestern University. She leads a translational research program focused on understanding HSV entry and pathogenesis, the HIV-HSV syndemic, and exploiting that knowledge to develop safe and effective antiviral therapies including vaccines and PrEP. Her team is studying intravaginal rings to protect women from HIV and HSV.
Debra Lesane
Ms. Lesane has more than 30 years of experience in the following areas of healthcare: strategic planning, program planning and development, and community affairs and advocacy. Ms. Lesane has worked in a variety of healthcare settings, including hospitals, mental health treatment organizations, and community-based organizations. Her career focus has been to develop health education programs and support services to underserved communities and to contribute to the overall elimination of health disparities in NYC. Ms. Lesane is the Director of Programs at the Caribbean Women’s Health Association, Inc. (CWHA), which is located in the Flatbush section of Brooklyn. CWHA provides a variety of services throughout NYC, including HIV testing and counseling, maternal and child health support programs, immigration legal assistance, and Medicaid/health insurance enrollment services. Ms. Lesane has recently been very involved in promoting community engagement in the implementation of the Delivery System Reform Incentive Payment Program in Brooklyn.
Johanne Morne, MS
Ms. Morne serves as Director of the NYS Health Department’s AIDS Institute, where she directs policy and program development related to HIV, hepatitis C, STDs, drug user health, and LGBTQ+ health. She has worked closely with community stakeholders in implementing the governor’s plan to end the AIDS epidemic in NYS by the end of 2020. Ms. Morne has bachelor’s degrees in psychology and social work and holds a master’s degree in education and counseling from the College of St. Rose. Before joining the Health Department, Ms. Morne directed community-based services at Whitney M. Young, Jr. Health Center, serving as clinical supervisor of chemical dependency services and program director of community outreach, mental health, and HIV services. At Albany Medical Center, Ms. Morne served as quality manager of psychiatry, behavioral health, and HIV services. She served as adjunct professor in the Sociology Department at the University of Albany for two years. Ms. Morne’s professional and clinical experience is in public health and behavioral health, particularly within communities of color.
Jaime Morrill
Ms. Morill is a PrEP Specialist from Rochester, New York. For the last year and a half she has worked at Trillium Health, first as a Retention and Adherence Specialist, and now, for almost a year, as a PrEP Specialist. Trillium Health is a neighborhood health center that specializes in LGBTQ+ services. While completing her bachelor’s degree in social work from SUNY Brockport, Jaime spent a year in Vietnam working with veterans and victims of Agent Orange. She then came to Trillium Health where her passion for helping others directed her at ETE 2020.
Maria Teresa (Tess) Timoney, CNM
Ms. Timoney is the Director of Women’s HIV Services for the Department of Obstetrics and Gynecology at Bronx Lebanon Hospital Center, where she has been providing obstetric and gynecological care for women with HIV infection since 2001. She has been actively involved in HIV prevention efforts throughout her career, from her role as a colposcopist for the HIV Prevention Trials Network Vaginal Microbicide Trials, to her current role as an investigator for IMPAACT. In 2016, she completed the Greater New York Hospital Association United Hospital Fund Clinical Quality Fellowship. She is currently working to implement expanded PrEP eligibility screening across the Bronx Lebanon Ambulatory Care Network. She attended the Columbia University School of Nursing and Barnard College. Before becoming a midwife, Ms. Timoney worked for many years is an artist and curator in New York City. She is most grateful to the women she has met and cared for in her practice at Bronx Lebanon.
Agenda with Links to Slides
- Welcome and Introductions:
Laura Duggan Russell, MPH, Senior Program Coordinator, Office of the Medical Director, NYSDOH AIDS Institute - Opening Remarks:
- Johanne Morne, MS, Director, NYSDOH AIDS Institute | View Slides
- Demetre Daskalakis, MD, Deputy Commissioner, Disease Control, NYC DOHMH | View Slides
PART I: INVITED SPEAKERS
The Conundrum of Topical and Systemic PrEP for Women: How to Deliver the Right Drugs to the Right Place at the Right Time | View Slides
Betsy C. Herold, MD, Professor of Pediatrics and Microbiology-Immunology, Vice Chair for Research in the Department of Pediatrics, and Division Chief, Pediatric Infectious Diseases at Albert Einstein College of Medicine and the Children’s Hospital at Montefiore, Bronx, NY
Beyond Condoms: Pre-Exposure Prophylaxis for Women During Preconception, Pregnancy, and Lactation | View Slides
Maria Teresa (Tess) Timoney, CNM, Director, Women’s HIV Services, Department of Obstetrics and Gynecology, Bronx Lebanon Hospital Center
“Is That for Me?”: Challenging Assumptions about PrEP for Women in the U.S. | View Slides
Dázon Dixon Diallo, MPH, DHL, Founder and President of SisterLove, Inc.
Questions & Answers
PART II: WORKING LUNCH WITH PANEL DISCUSSION
Real-World Experiences in Implementing PrEP for Women
- Jamie Morrill, PrEP Specialist, Trillium Health | View Slides
- Debra Lesane, Program Director, Caribbean Women’s Health Association, Inc. | View Slides
- Kate Collier, PhD, MPH, Director of Research & Evaluation, Planned Parenthood of New York City
Questions & Answers
PART III: ROUND-ROBIN BREAKOUT SESSIONS
Participant Discussions: Attendees will circulate through three 25-minute breakout sessions to discuss their experiences with the following key topics in PrEP implementation for women: awareness of PrEP, perception of risk for HIV, and access to PrEP. After 25 minutes of discussion in one session, participants will be directed to the next session until everyone has had the opportunity to participate in each of the three sessions. After a short break, we will gather to report out and identify priorities for policy and change.
PART IV: PRIORITIES FOR POLICY AND CHANGE: REPORTS FROM BREAKOUT SESSIONS
Report Out: Successes, Challenges, and Priorities for Change
Session leaders will report out to the whole group with the goal of identifying the top 3-5 items in each of the following areas:
- Issues and challenges unique to PrEP implementation for women
- Keys to success, including best practices for engaging women
- Policies needed to increase PrEP uptake among women
- Priorities for change to guarantee success in the next 3 years
- Based on concerns and solutions identified are there suggested policy changes/program changes/interventions?
Next Steps and Closing Remarks: Laura Duggan Russell
Resources
Posted October 18, 2017
Resources
- PrEPforSex.org
- HIVE Blog “Share Your Story”
- U.S. Women & PrEP Working Group: Please send any questions or comments here
- SisterLove, Inc.
- Project Inform: PrEP
- NYSDOH AIDS Institute Provider Directory
- New York State Department of Health PrEP-AP Participating Provider Directory
- Please PrEP Me – National PrEP Directory
PrEP for Transgender Women
October 2018
This forum was the fourth in a series and a continuation of efforts to engage community and policy stakeholders in support of Governor Andrew Cuomo’s plan to end the HIV epidemic in New York State. A key component of the governor’s plan is to increase access to and uptake of PrEP among people who are at high risk of acquiring HIV infection.
PrEP implementation for adults was addressed on August 26, 2015, when the New York State Department of Health AIDS Institute (NYSDOH AI) convened a forum, attended by healthcare providers, consumers, community stakeholders, and state and local health officials, to discuss the use of PrEP and PrEP quality of care for adults in New York State. On November 18, 2015, a forum on implementation of adolescent PrEP was convened to address challenges and opportunities specific to the youth population. The third in the series, PrEP for Women, focused on identifying challenges that must be addressed to increase women’s access to PrEP and their willingness to use it to protect themselves from acquiring HIV.
Available materials from the PrEP for Transgender Women Meeting:
- Meeting Summary Report
- Agenda
- Speaker Presentations (with links to slides)
- Speaker Bios
- Breakout Session Guidance
Challenges Unique to Transgender Women
Among presenters, panelists, and meeting participants, there was broad agreement that transgender women in New York State are particularly vulnerable to HIV and particularly in need of access to PrEP. Speakers noted the steady increase in new diagnoses of HIV among transgender women, particularly among transgender women of color and younger transgender women.
Key Issues and Priorities for Change
All acknowledged that issues of social oppression, discrimination, and inadequate service delivery pose the greatest challenges in improving access to and uptake of PrEP among transgender women in NYS. Toward that end, participants stressed the importance of ending institutionalized transphobia and embracing the reality that a transgender person is entitled to the same quality of care as all other people. That focus is reflected in the key issues and priorities for change identified by meeting participants.
1. Improve care and service delivery environments to expand access to PrEP for transgender women:
- Ensure cultural competency among all who interact with transgender women so they can expect safe, gender-affirming care always.
- Increase funding for transgender-centered services and expand the number and diversity of settings that provide PrEP and other healthcare for transgender women.
- Increase opportunities for transgender people to work in care- and service-delivery settings and foster commitment to hiring and training transgender people for this type of work.
- Create marketing and messaging specifically designed to reach transgender women.
2. Reduce social oppression, discrimination, and stigmatization to increase uptake of PrEP among transgender women:
- Enforce anti-discrimination laws already in place to protect the rights of transgender people; facilitate passage of new laws that offer further protection.
- Tailor services to meet the social, economic, and healthcare needs of transgender women; PrEP will not be a priority for transgender women in need of housing and food security, transportation, and basic healthcare.
- Decriminalize sex work and protect sex workers’ rights. Sex work is survival for transgender women and others who face social and structural barriers to employment.
- Focus on occupational safety in discussions of PrEP; HIV risk is an occupational hazard for sex workers.
3. Improve awareness and knowledge of transgender women’s healthcare needs:
- Require training in best practices in care of transgender women for all medical care providers.
- Offer non-clinical care in the same settings as clinical care, as wrap-around services.
- Promote research on PrEP efficacy in transgender women.
- Bundle hormone therapy with PrEP, always.
- Expand advertising, education, and payment options for PrEP and ensure that all campaigns and materials are transgender inclusive.
Summary Report
October 2018
This report summarizes speaker presentations and panel and participant discussions at the first statewide forum on PrEP implementation for transgender women in New York. This meeting was hosted by the New York State Department of Health AIDS Institute (NYSDOH AI) on April 10, 2018.
Speaker Bios
October 2018
Johanne Morne, MS
Ms. Morne currently serves as Director of the New York State Department of Health (NYS DOH) AIDS Institute. The AIDS Institute has a broad mission including hepatitis and sexually transmitted disease (STD) services, surveillance, opioid overdose prevention, and non-HIV Lesbian, Gay, Bisexual, and Transgender (LGBT) services into its structure. The AIDS Institute formulates policy related to HIV, hepatitis, STDs, drug user health, and LGBT health and human services; initiates, develops, and evaluates programs for the delivery of HIV, hepatitis, and STD prevention, healthcare and supportive services as well as drug user health and LGBT health and human services; establishes clinical standards and oversees quality management; educates healthcare providers and the public; and guides regional and statewide planning. In its more than 30-year history, the AIDS Institute has provided leadership in NYS, at the national level, and internationally. Ms. Morne’s leadership advanced the State’s deliberations related to Undetectable=Untransmittable and led the NYS DOH to sign on to the U=U consensus statement. New York was the first state to do so. Ms. Morne currently serves as a board member of the National Alliance of State and Territorial AIDS Directors (NASTAD). Ms. Morne is also an honoree in the 2017 POZ 100: Celebrating Women. Prior to joining the State Health Department, Ms. Morne served as quality manager of psychiatry and HIV services at a Designated AIDS Center hospital and director of community-based HIV services at a federally qualified health center. Ms. Morne’s professional and clinical experience is in public health and behavioral health, particularly within communities of color.
Oni Blackstock, MD
Dr. Blackstock is Assistant Commissioner for the New York City Department of Mental Health and Hygiene’s Bureau of HIV/AIDS Prevention and Control. She is a primary care physician, HIV specialist, and researcher who has developed, implemented, and evaluated innovative community and clinic-based programs to promote HIV treatment and prevention. Dr. Blackstock is at the forefront of local efforts to increase access and uptake of biomedical HIV prevention technologies among cis and trans women who engage in transactional sex or inject drugs. She received her undergraduate and medical degrees from Harvard University, and her MHS from Yale School of Medicine in the Robert Wood Johnson Foundation Clinical Scholars Program. She trained in primary care internal medicine at Montefiore Medical Center in the Bronx and completed a fellowship in HIV medicine at Harlem Hospital.
Gus Klein, MSW
Gus Klein is a doctoral candidate in Social Welfare at the CUNY Graduate Center and a research associate at the Hunter HIV/AIDS Research Team. He conducts community-based participatory research on health disparities in the transgender and non-binary communities. He is also a social worker who has been working with diverse communities in a variety of settings for the past 20 years.
Asa Radix, MD, MPH, FACP
Dr. Radix is the Senior Director of Research and Education at the Callen-Lorde Community Health Center and a Clinical Associate Professor of Medicine at New York University. Dr. Radix has over 20 years of experience providing HIV care, primary care, and hormone therapy to transgender and gender non-binary people. Dr. Radix has contributed to multiple national and international guidelines in transgender health and is currently Co-Chair of the World Professional Association of Transgender Health (WPATH) Standards of Care version 8 working group and a member of the HHS Panel on Antiretroviral Guidelines for Adults and Adolescents.
Zil Goldstein, FNP-BC
Zil Goldstein is an Assistant Professor of Medical Education at the Icahn School of Medicine and the Program Director at the Center for Transgender Medicine and Surgery at Mount Sinai. She has served as a clinical specialist in transgender and HIV health at multiple institutions, and, with over 10 years of experience in managing the healthcare of transgender individuals, has played an instrumental role in building transgender services throughout the Mount Sinai Health System.
Melanie Dulfo, LMSW
Melanie Dulfo started as a Peer Educator in HIV prevention and is now the Director for Community Health Education at Apicha CHC. She launched linkage and navigation services for Apicha CHC’s HIV prevention projects, including linking and coordinating clients to PrEP treatment and has learned many lessons in integrating services, from outreach to retaining people in care.
Timothy Au, LMSW
Timothy Au, Program Manager for Support Services, assists the Support Services department in overseeing of programs implementation, including supervision of the PrEP navigation services and Trans Health Care Services. Mr. Au holds a Master’s degree in Social Work and has obtained license from the New York State Board of Education as a Licensed Master Social Worker. Mr. Au has over 7 years’ experience in case management of clients living with HIV/AIDS as well as managing case management services.
La’Mia White-Revlon Aiken
Also known as Mother, La’Mia White-Revlon is the Voice for her fellow brothers and sisters. From her humble beginning over 20 years ago in church serving as a youth Minister as a teen, leading up to her service as an Elder as an adult, La’Mia has always been determined not only to be visible but vocal for her peers’ rights to be heard. Upon entering the LGBT community in 2004 she founded The House of Encore. The House of Encore would be the platform in which La’Mia would use to reach a target population desperately in need representation. With the goal of making a meaningful difference, La’Mia joined forces with In Our Own Voices, where she started off as volunteer and worked her way up to a Peer Educator, Facilitator for “T-SISTA,” and Ball Promoter for our annual Black and Latino Gay Pride. Now as a full-time employee, to date La’Mia is continuing with her passion by getting involved in issues surrounding transgender equality and awareness and HIV/AIDS prevention. She is working diligently to end the HIV/AIDS epidemic by 2020 in NYS.
Agenda with Links to Slides
- Welcome and Introductions:
Laura Duggan Russell, MPH, Senior Program Coordinator, Office of the Medical Director, NYS DOH AIDS Institute - Opening Remarks:
- Johanne Morne, Director, NYS DOH AIDS Institute | View Slides
- Oni Blackstock, MD, Assistant Commissioner, Bureau of HIV/AIDS Prevention and Control, NYC DOHMH | View Slides
PART I: INVITED SPEAKERS
Facilitators and Barriers to PrEP Among Transgender Women in New York City | View Slides
Gus Klein, MSW, Hunter HIV/AIDS Research Team
Sexual Health for Transgender Women | View Slides
Asa Radix, MD, MPH, FACP, Senior Director of Research and Education, Callen-Lorde Community Health Center; Clinical Associate Professor of Medicine at New York University
Gender-Affirming Clinical Care for Transgender Women
Zil Garner Goldstein, FNP-BC, Assistant Professor of Medical Education; Program Director,
Center for Transgender Medicine and Surgery at Mount Sinai
Questions & Answers
PART II: WORKING LUNCH WITH PANEL DISCUSSION
Real-World Experiences in Implementing PrEP for Transgender Women
- Melanie Dulfo, LMSW, Director of Community Health Education, Apicha Community Health Center, New York, New York & Timothy Au, LMSW, Program Manager for Support Services, Apicha CHC, NY, NY | View Slides
- La’Mia Aiken, TransCare Advocate, In Our Own Voices, Albany, New York | View Slides
Questions & Answers
PART III: ROUND-ROBIN BREAKOUT SESSIONS
Participant Discussions: Attendees will circulate through three 25-minute breakout sessions to discuss their experiences with the following key topics in PrEP implementation for transgender women: 1) Access to PrEP; 2) PrEP Retention; 3) PrEP Public Health Program Design. After 25 minutes of discussion in one session, participants will be directed to the next session until everyone has had the opportunity to participate in each of the three sessions. After a short break, we will gather to report out and identify priorities for policy and change.
PART IV: PRIORITIES FOR POLICY AND CHANGE: REPORTS FROM BREAKOUT SESSIONS
Report Out: Successes, Challenges and Priorities for Change
Session leaders will report out to the whole group with the goal of identifying the top 3-5 items in each of the following areas:
- Issues and challenges unique to PrEP implementation
- Keys to success, including best practices for engagement
- Policies needed to increase PrEP uptake
- Priorities for change to guarantee success in the next 3 years
- Based on concerns and solutions identified are there suggested policy changes/program changes/interventions?
Next Steps and Closing Remarks: Laura Duggan Russell
Resources
October 2018
- UCSF Center of Excellence for Transgender Health
- National LGBT Health Education Center
- Project Inform
- Ending the Epidemic
- Clinical Training Initiative
- NYSDOH AI HIV Education & Training Programs
PrEP/PEP Directories

